Table of Contents
ToggleC-Peptide Test Explained Simply
Discover what the C-peptide test is, why it’s used to measure natural insulin production, and how it helps distinguish type 1 and type 2 diabetes or investigate low blood sugar. Easy-to-understand guide for everyone.
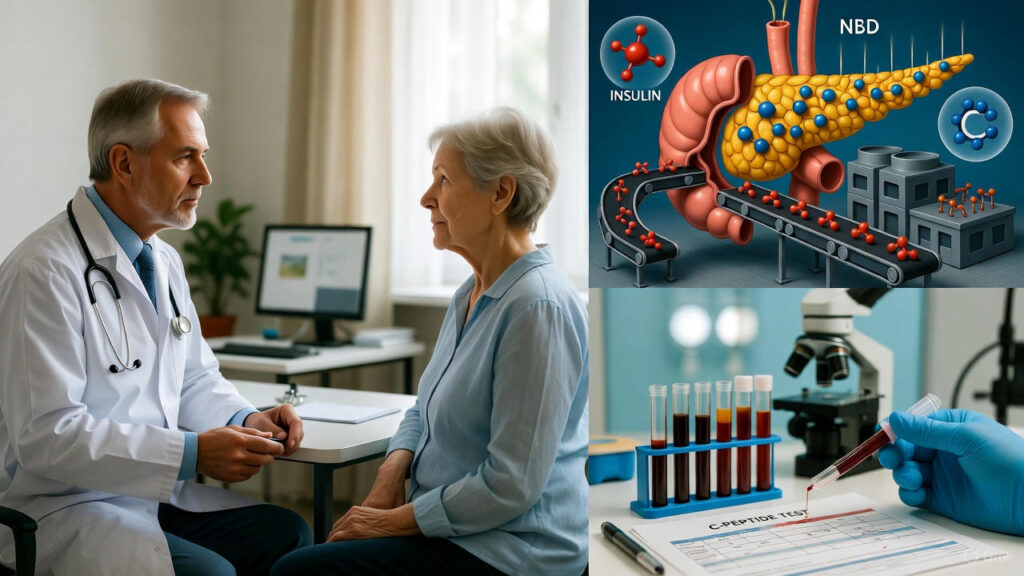
Understanding the C-Peptide Test: A Window into Your Body’s Insulin Factory
Imagine your pancreas as a busy factory deep inside your body, quietly producing one of the most vital hormones: insulin. Insulin acts like a key, unlocking cells so they can absorb sugar (glucose) from your blood for energy. Without enough insulin, blood sugar levels rise, leading to diabetes and other health issues.
But here’s a fascinating twist—insulin doesn’t come out of the factory alone. It’s born as a larger molecule called proinsulin, which gets split into two parts: the active insulin and a byproduct called C-peptide (short for “connecting peptide,” because it literally connects the pieces in proinsulin).
When your pancreas releases insulin, it releases an equal amount of C-peptide. Unlike insulin, which can be quickly cleared from the blood (especially if you’re injecting it for treatment), C-peptide lingers longer and isn’t affected by external insulin shots. This makes the C-peptide test a reliable “spy” for measuring how much insulin your own body is naturally producing.
Why Do Doctors Order a C-Peptide Test?
This simple blood test (sometimes done on urine) helps answer key questions about your health:
- Distinguishing Types of Diabetes
– In Type 1 diabetes, the immune system attacks the pancreas’s insulin-producing cells (beta cells). Over time, the factory shuts down, leading to very low or undetectable C-peptide levels.
– In Type 2 diabetes, the body often makes plenty of insulin at first (high C-peptide), but cells become resistant to it. Later, the pancreas may tire out, and levels can drop.
Knowing your C-peptide helps guide treatment—whether you need insulin injections right away or can start with lifestyle changes and oral medications.
- Investigating Low Blood Sugar (Hypoglycemia)
If your blood sugar drops too low without an obvious reason (like skipping meals), high C-peptide could point to:
– An insulinoma (a rare, usually benign tumor in the pancreas that overproduces insulin).
– Or, rarely, overuse of certain medications.
Low C-peptide with low sugar might suggest other causes, like liver issues or external insulin use.
- Monitoring Treatment Progress
For people with diabetes on insulin therapy, C-peptide shows if your pancreas is still contributing any natural insulin. It can help decide if new medications (like GLP-1 agonists) are boosting your own production or if it’s time to adjust therapy.
- Other Rare Uses
It can check pancreas function after surgery, transplants, or in conditions like Cushing’s syndrome.
What Happens During the Test?
It’s straightforward—like a routine blood draw.
– You may need to fast for 8–12 hours (no food, just water).
– Sometimes, it’s done after a meal or a “stimulation” test (e.g., with glucagon) to see how your pancreas responds.
– A small needle draws blood from your arm—no big deal for most people!
Interpreting Results: What Do the Numbers Mean?
Normal fasting C-peptide levels are roughly 0.8–3.9 ng/mL (or 0.26–1.3 nmol/L), but labs vary slightly—always check your report’s reference range.
Results are always interpreted with your blood sugar, symptoms, and history. For example:
– High C-peptide + high sugar = Likely Type 2 (insulin resistance).
– Low C-peptide + high sugar = Likely Type 1 (insulin deficiency).
– High C-peptide + low sugar = Possible overproduction (e.g., tumor).
Why This Test Matters for Your Health Journey
A specialist physician told me that “in my 15 years as an endocrinologist, I’ve seen the C-peptide test change lives. It clarifies confusing diagnoses, prevents unnecessary treatments, and gives hope—showing if some natural insulin production remains”. For someone newly diagnosed with diabetes, it can mean starting with pills instead of shots, or vice versa.
If your doctor suggests this test, it’s a positive step toward personalized care. Diabetes management has advanced tremendously; understanding your body’s own insulin story empowers better control and a healthier future.
Conclusion
Always discuss results with your healthcare provider—they’ll connect the dots for your unique situation. Stay curious about your health—it’s the best way to thrive!